GENEVA, Switzerland – To accelerate identification, guaranteeing prompt treatment, and enhancing long-term care for individuals afflicted, the World Health Organisation (WHO) released its first-ever global guidelines for meningitis diagnosis, treatment, and care this week.
The guidelines offer a vital tool for lowering disease-related mortality and disability by compiling the most recent evidence-based recommendations.
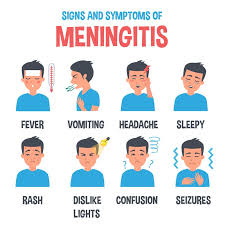
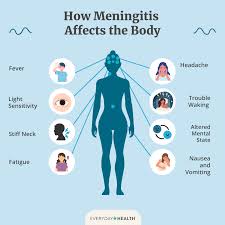
Even with efficient therapies and vaccinations to prevent some types of meningitis, the illness continues to pose a serious risk to world health. The most severe type, bacterial meningitis, can be lethal in as little as 24 hours.
Meningitis can be caused by a variety of pathogens; in 2019, an estimated 2.5 million cases were recorded worldwide. Approximately 240,000 people died as a result of 1.6 million cases of bacterial meningitis.
About 20% of patients who get bacterial meningitis go on to experience long-term problems, such as impairments that lower their quality of life. Additionally, the illness has significant social and economic repercussions for people, families, and communities.
“One in six victims of bacterial meningitis die from the disease, and many more suffer from long-term health problems, according to WHO Director-General Dr. Tedros Adhanom Ghebreyesus. ” Implementing these new guidelines will help save lives, improve long-term care for those affected by meningitis, and strengthen health systems.”
10.4.25 New @WHO Guidelines on #Meningitis, a devastating disease that can be deadly & often results in serious Long-term Health issues who.int/health-topics/… @Concern @ifglobalhealth @RCSI_Irl @ConcernMalawi @BdConcern @ConcernKenya @INMO_IRL @Irish_Aid @emranul @edwin_mbugua
Although meningitis can strike anybody, anywhere, and at any age, the illness burden is still highest in low- and middle-income nations and in areas where widespread outbreaks are occurring. A region of sub-Saharan Africa known as the “meningitis belt” has the highest disease burden and is particularly vulnerable to recurring meningococcal meningitis outbreaks.
Recommendations for the clinical management of meningitis in children and adults
Reducing mortality and morbidity, minimising long-term consequences and disability, and enhancing the quality of life for afflicted individuals and communities all depend on better therapeutic management of meningitis.
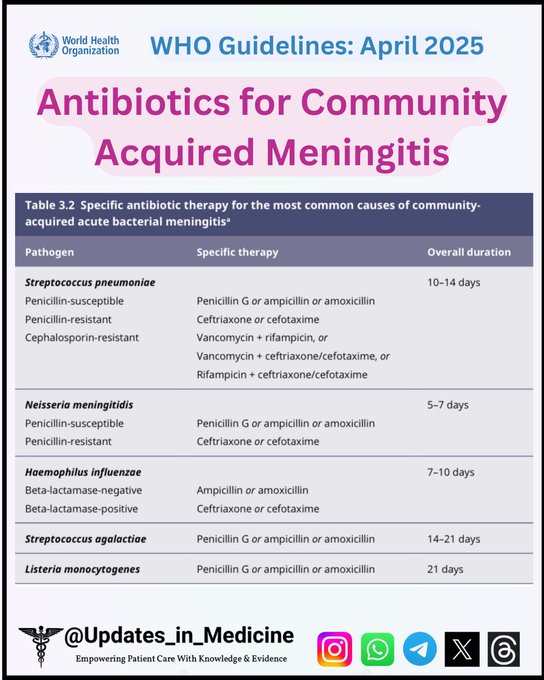
The updated guidelines include evidence-based suggestions for the clinical treatment of acute community-acquired meningitis in adults, adolescents, and children older than one month.
They cover every facet of clinical care, such as supportive care, adjuvant treatment, antibiotic therapy, diagnosis, and long-term effect management. The guidelines cover both bacterial and viral causes of acute community-acquired meningitis because of the parallels in clinical presentation, diagnosis, and therapeutic strategies among various types of the illness.
The 2014 WHO guidelines, which addressed meningitis outbreak response, have been replaced by the guidelines, which offer guidance for both non-epidemic and epidemic contexts.
Since meningitis is most common in settings with little resources, these guidelines were created especially to offer technical advice that can be used in low- and middle-income nations.
Health care providers working in first- and second-level facilities, including emergency, inpatient, and outpatient services, are supposed to utilise the guidelines. They can also be used by academic institutions, civil society organisations, policymakers, and health planners to guide research, education, and capacity-building initiatives.
Defeating meningitis by 2030
The guidelines contribute to the broader Defeating Meningitis by 2030 Global Roadmap, adopted by WHO Member States in 2020, which aims to eliminate bacterial meningitis epidemics, reduce cases of vaccine-preventable bacterial meningitis by 50% and deaths by 70%, and reduce disability and improve quality of life after meningitis.
Achieving these goals requires coordinated action across five key areas:
- Diagnosis and treatment: Faster detection and optimal clinical management.
- Prevention and epidemic control: Developing new affordable vaccines, achieving high immunisation and coverage, and improving outbreak preparedness and response.
- Disease surveillance: Strengthening monitoring systems to guide prevention and control.
- Care and support for those affected by meningitis: Ensuring early recognition and improved access to care and support for after-effects from meningitis.
- Advocacy and engagement: Increasing political commitment and inclusion in country plans, better public understanding of meningitis, and increased awareness of the right to prevention, care, and after-care services.
WHO April 2025: Antibiotics for community-acquired meningitis—duration ranges 5–21 days. Tailor therapy to pathogen & resistance. #medtwitter #IDtwitter #WHOguidelines #updatesinmedicine
With these guidelines, WHO provides countries with a critical tool to close gaps in meningitis diagnosis, treatment, and care, ensuring that more people receive timely treatment and long-term support.